Overview
The article outlines seven essential strategies for effective healthcare turnaround management, emphasizing the importance of comprehensive assessments, strong leadership, stakeholder engagement, and strategic planning to navigate financial and operational challenges. These strategies are supported by case studies and statistics that demonstrate their effectiveness in improving clinical performance, operational efficiency, and financial stability, ultimately leading to sustainable success in healthcare organizations.
Introduction
In the face of unprecedented challenges, healthcare organizations are at a critical juncture where effective turnaround management is not just desirable but essential for survival. With rising operational costs, shifting patient expectations, and increasing regulatory pressures, leaders must adopt foundational principles that pave the way for sustainable success.
This article delves into practical strategies that healthcare executives can implement to optimize operational efficiency, engage stakeholders, and measure the impact of their turnaround initiatives.
By embracing these actionable insights, organizations can not only navigate financial turbulence but also enhance patient care and foster a resilient healthcare system for the future.
Foundational Principles of Healthcare Turnaround Management
Several essential principles anchor effective healthcare turnaround management, guiding organizations through challenging times. First, conducting a comprehensive assessment of the current operational and economic landscape is paramount. This process includes scrutinizing financial statements, analyzing patient flow, and evaluating resource allocation to pinpoint critical areas requiring attention.
Statistics reveal that the five lowest-performing states for health system performance—Mississippi, West Virginia, Oklahoma, Texas, and Arkansas—highlight the need for urgent corrective measures.
Second, unwavering leadership commitment is crucial. Strong leaders possess the ability to instigate cultural transformations within their institutions, fostering an environment receptive to change. As reported by Ultimate Medical Academy, a nationwide study found that 1 in 5 employees in support roles left their positions in the past six months, underscoring the necessity for robust leadership to retain talent and maintain operational continuity.
The case study 'Achieving Sustainability' illustrates this point, demonstrating that by improving clinical and operational performance, hospitals can avoid the drastic measure of divestment. This case study emphasizes the importance of leadership engagement in rallying stakeholders and driving necessary changes, ultimately leading to a successful turnaround.
Third, engaging stakeholders—including staff, patients, and suppliers—promotes collaboration and secures buy-in for proposed changes. This inclusive approach helps to create a shared vision and enhances the likelihood of successful implementation.
Additionally, a clear and strategic plan must be articulated, detailing the desired outcomes and actionable steps necessary to achieve them. Moreover, implementing streamlined decision-making processes and utilizing real-time analytics will enable businesses to monitor performance continuously. This commitment to operationalizing lessons learned throughout the recovery process fosters strong, lasting relationships with stakeholders.
Importantly, testing hypotheses at every stage ensures maximum return on invested capital, allowing for informed adjustments. By adhering to these foundational principles, medical organizations can lay the groundwork for successful healthcare turnaround management initiatives. These strategies not only maintain the fundamental mission of hospitals during financial crises but also contribute to the overall stability of community medical systems.
The journey may be lengthy and fraught with challenges; however, the pursuit of improved clinical and operational performance, rather than divestment, can ultimately lead to sustainable success. Furthermore, recent trends highlighted by the AMN Healthcare survey indicate a decline in registered nurses' career satisfaction, emphasizing the importance of effective leadership in fostering a supportive work environment that retains skilled professionals. The urgency of a shortened decision-making cycle allows teams to take decisive action, ensuring that turnaround efforts are both timely and effective.
Key Strategies for Enhancing Operational Efficiency in Healthcare
To significantly enhance operational efficiency in the medical field and master the cash conversion cycle, organizations can adopt several pivotal strategies from the 'Mastering the Cash Conversion Cycle: 20 Strategies for Optimal Business Performance':
- Streamlining Processes: A comprehensive analysis of workflows is essential to pinpoint bottlenecks and redundancies. Implementing Lean methodologies is a crucial aspect of healthcare turnaround management, as it can effectively eliminate waste and optimize patient flow. SSM Health's new operating model, based on Lean management principles, emphasizes hands-on leadership to improve quality and reduce infection rates, showcasing the real-world effectiveness of these strategies in enhancing business performance.
- Utilizing Technology: Investing in advanced health information technology systems is crucial for improving data management, enhancing communication, and facilitating telemedicine services. Such investments not only boost operational efficiency but also foster patient engagement, which is essential for optimizing cash flow. For instance, studies indicate that when care includes physician assistants, patients experience 16% fewer office-based visits compared to those who receive care solely from physicians, as noted by healthcare expert Perri Morgan. This emphasizes the importance of incorporating technology and support personnel in improving patient care and, ultimately, economic performance.
- Monetary Management: Robust oversight practices, including budgeting, forecasting, and cash flow management, are vital for ensuring economic stability. Routine fiscal evaluations are crucial in identifying and correcting inefficiencies, enabling medical organizations to sustain economic well-being while concentrating on operational enhancements. The efficiency analysis of 19 tertiary hospitals in Taiwan revealed an average technical efficiency of 96.0% in the CCR model and 99.1% in the BCC model, underscoring the importance of economic management in achieving operational excellence and mastering the cash conversion cycle.
- Workforce Optimization: Assessing staffing levels and the skill sets of medical professionals is critical. Ensuring that the right personnel are in place, coupled with targeted training and development programs, enhances employee capabilities and service delivery. This approach aligns with findings from the efficiency analysis of tertiary hospitals in Taiwan, where healthcare turnaround management has demonstrated that technical efficiency increased annually, underscoring the importance of human resources in operational success and performance improvement.
- Patient-Centric Care: Transitioning to a patient-centered approach fosters greater involvement of patients in their care plans, leading to enhanced outcomes and increased satisfaction. This strategic change not only enhances patient experiences but also positively impacts operational metrics and economic performance.
By strategically applying these methods, medical entities can significantly boost their operational efficiency and master the cash conversion cycle, ultimately resulting in improved economic results and superior patient care. For more insights and to explore the complete list of 20 strategies, consider investing in our comprehensive guide available for $99.00.
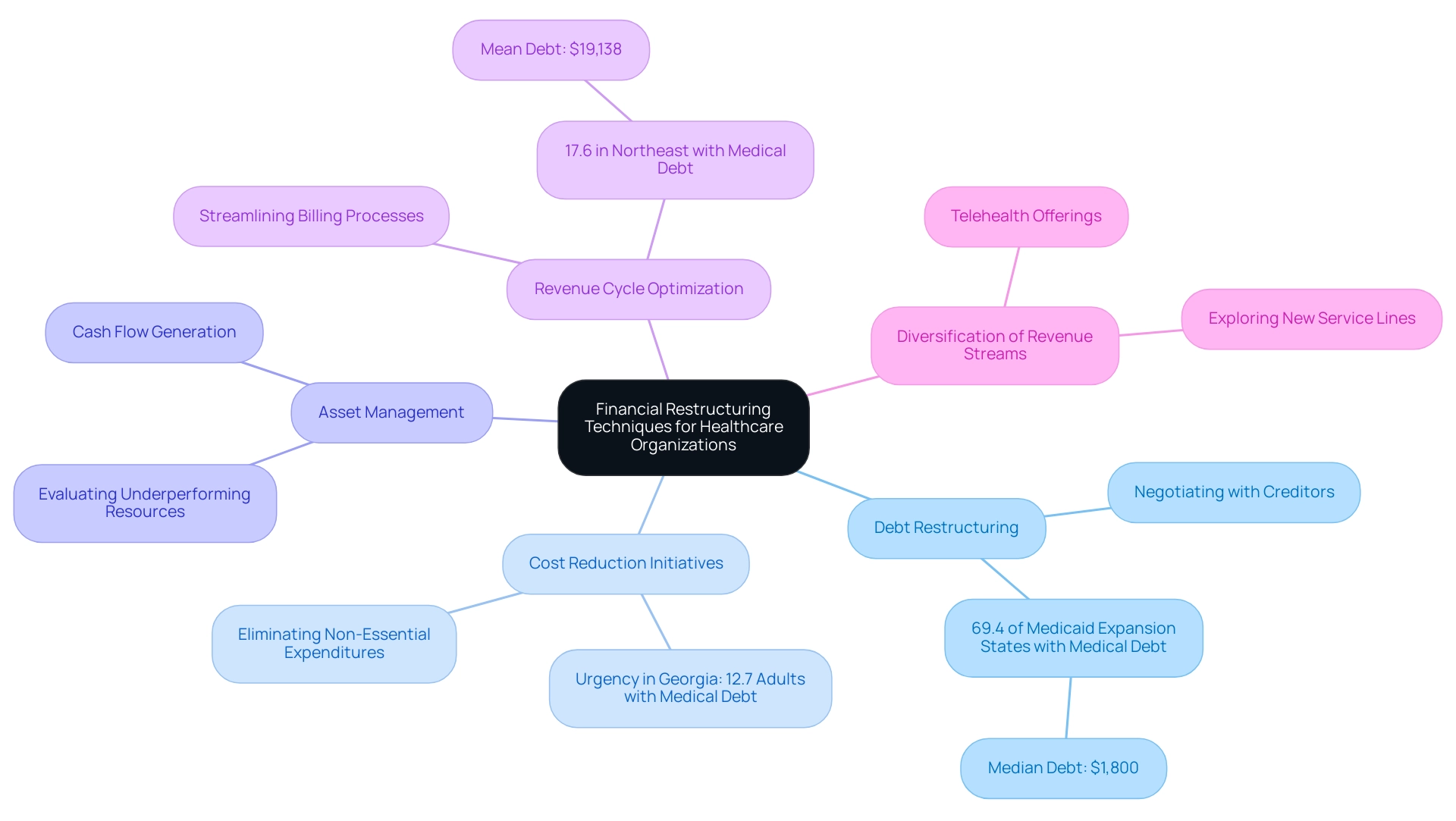
Financial Restructuring Techniques for Healthcare Organizations
Financial restructuring in healthcare organizations encompasses several critical techniques aimed at improving fiscal health and operational efficiency:
- Debt Restructuring: Engaging with creditors to negotiate terms can significantly alleviate monetary burdens. This may involve securing reductions in interest rates or extending payment periods, which is particularly crucial given that 69.4% of individuals in Medicaid expansion states are burdened with medical debt, averaging a median of $1,800. Adam Gaffney highlights the importance of such restructuring efforts, stating, "The economic environment requires that healthcare entities embrace innovative strategies to manage their debts effectively."
- Cost Reduction Initiatives: Identifying and eliminating non-essential expenditures is vital. Implementing cost-reducing strategies—such as renegotiating agreements with suppliers or minimizing overhead expenses—ensures that patient care quality remains uncompromised while improving economic sustainability. In Georgia, where 12.7% of adults report medical debt, these initiatives are particularly urgent.
- Asset Management: A thorough evaluation of assets can reveal underperforming resources that may be sold or leased. This method produces cash flow that can be reinvested into core operations, further stabilizing the entity’s economic position.
- Revenue Cycle Optimization: Streamlining billing and collection processes is essential for enhancing cash flow. Prompt and precise billing, along with thorough follow-ups on unpaid claims, can significantly enhance economic results. With 17.6% of individuals in the Northeast reporting medical debt, this technique is crucial for organizations operating in that region.
- Diversification of Revenue Streams: Exploring new service lines or partnerships can create additional revenue channels. Outpatient services and telehealth offerings are prime examples of revenue diversification that can enhance economic resilience.
Statistics highlight the pressing nature of these strategies, especially in regions like the Northeast, where 17.6% of individuals report medical debt, with a mean debt of $19,138. The economic pressure on medical facilities is clear, as demonstrated by the case studies of prominent hospitals like John Peter Smith and Grady Memorial, which reported bad debt amounts between $3.2 million and $5.47 million. By utilizing these financial restructuring methods, medical entities can implement healthcare turnaround management to stabilize their finances and strategically position themselves for long-term success in an increasingly challenging landscape.
Engaging Stakeholders in the Turnaround Process
Effectively involving stakeholders throughout the transformation process is crucial for attaining desired results in healthcare turnaround management. Here are key strategies that can be implemented:
- Transparent Communication: Consistently update all stakeholders on the recovery objectives, progress, and challenges. This fosters trust and collaboration, which are crucial for overcoming resistance and ensuring alignment. As Andrew T. Herndon, Senior Business Manager at The University of Texas Medical Branch, states, "Serving the Traditionally Underserved with Population Health Improvements" highlights the critical role of effective communication in addressing the needs of diverse populations.
- Involvement in Decision-Making: Actively involve key stakeholders—including staff and department heads—in the decision-making process. Our team supports a shortened decision-making cycle throughout the healthcare turnaround management process, enabling your company to take decisive action to preserve business health. Their insights and concerns are invaluable for crafting effective solutions that resonate with the needs of the organization. Notably, children under the age of 5 years are identified as being at high risk for medication errors related to incorrect dose adjustments, emphasizing the necessity of engaging relevant stakeholders in healthcare settings to mitigate such risks.
- Building a Change Management Team: Form a dedicated change management team composed of representatives from various departments. This diverse group ensures that a broad range of perspectives is considered, enhancing the comprehensiveness of the recovery strategy. The case study on stakeholder engagement in genomics policy illustrates how integrating stakeholder input is crucial for developing effective public health policies.
- Feedback Mechanisms: Establish robust channels for stakeholders to provide feedback on improvement initiatives. We continually monitor the success of our plans through our client dashboard, which provides real-time business analytics to assess your company's health. This enables quick adjustments based on their insights, thus increasing the initiatives' effectiveness and relevance.
- Recognition and Incentives: Acknowledge and reward stakeholders who positively contribute to improvement efforts. This approach fosters a culture of collaboration and commitment, motivating others to actively participate in the process.
By prioritizing stakeholder involvement and executing these strategies, medical entities can foster a supportive atmosphere, significantly improving the chances of successful recovery results through effective healthcare turnaround management.
Measuring Success in Healthcare Turnaround Initiatives
To effectively assess the success of healthcare recovery initiatives, entities must concentrate on several essential key performance indicators (KPIs) that promote improvement and accountability:
- Economic Indicators: Consistently tracking fluctuations in income, profit margins, and cash flow is crucial to evaluate the economic well-being of the organization after applying recovery strategies. For instance, the 'Revenue per Patient' case study illustrates how this indicator helps hospital operations professionals assess financial performance, identifying potential for revenue development and the institution's financial health.
- Operational Efficiency: Key indicators like patient wait times, completion time for tasks such as processing lab tests or admitting patients, staff productivity, and resource utilization should be tracked to evaluate improvements in operational performance. Streamlining these processes can lead to significant enhancements in service delivery, enabling a more agile response to operational challenges.
- Patient Satisfaction: Conducting comprehensive surveys to gauge patient satisfaction and engagement is crucial. This guarantees that the quality of care stays a top priority during the recovery process, ultimately fostering loyalty and positive outcomes. Continuous feedback allows organizations to adjust strategies in real time, reinforcing strong patient relationships.
- Staff Engagement: Regular feedback and surveys should be employed to assess employee morale and engagement levels. A motivated workforce is essential for the successful execution of transformation initiatives; understanding their viewpoints drives continuous enhancement. Empowering staff through transparent communication enhances their commitment and contributions.
- Compliance and Risk Management: Maintaining adherence to regulatory standards is non-negotiable. Monitoring adherence and effective risk management practices can help mitigate potential issues that may occur during the change. Proactive assessment through real-time analytics supports informed decision-making and strengthens organizational resilience.
By consistently measuring these KPIs, healthcare entities can validate the effectiveness of their turnaround efforts and make informed adjustments to optimize outcomes. Emphasizing streamlined decision-making and real-time analytics is crucial for CFOs looking to enhance overall organizational performance. Additionally, identifying underlying issues through collaborative planning and testing hypotheses can significantly improve the success of these initiatives. Ready to elevate your organization's performance? Book a personalized demo today!
Conclusion
Navigating the complexities of healthcare turnaround management requires a multifaceted approach grounded in strategic principles. By conducting thorough assessments of operational and financial landscapes, leaders can uncover critical areas for improvement. The commitment to strong leadership is essential in driving cultural transformations and ensuring stakeholder engagement, which fosters collaboration and aligns efforts toward shared goals.
Implementing key strategies such as:
- Streamlining processes
- Leveraging technology
- Optimizing financial management
can significantly enhance operational efficiency. These tactics not only improve the cash conversion cycle but also reinforce patient-centered care, ultimately leading to better financial performance and outcomes. Furthermore, financial restructuring techniques, including:
- Debt management
- Revenue cycle optimization
are vital for stabilizing organizations amid financial pressures.
Engaging stakeholders through transparent communication and inclusive decision-making is paramount for successful turnaround initiatives. Establishing feedback mechanisms and recognizing contributions cultivates a supportive environment that enhances collaboration and commitment.
Finally, measuring success through critical performance indicators enables organizations to assess their progress and make informed adjustments. By focusing on:
- Financial metrics
- Operational efficiency
- Patient satisfaction
- Staff engagement
- Compliance
healthcare executives can validate their strategies and drive sustainable success. Embracing these actionable insights empowers healthcare organizations to not only survive but thrive in an increasingly challenging environment, ensuring improved patient care and a resilient future.
Frequently Asked Questions
What are the essential principles of effective healthcare turnaround management?
The essential principles include conducting a comprehensive assessment of the operational and economic landscape, ensuring unwavering leadership commitment, engaging stakeholders, articulating a clear strategic plan, implementing streamlined decision-making processes, and testing hypotheses at every stage.
Why is conducting a comprehensive assessment important in healthcare turnaround management?
A comprehensive assessment helps organizations scrutinize financial statements, analyze patient flow, and evaluate resource allocation to identify critical areas that require attention, which is vital for effective turnaround management.
What role does leadership play in healthcare turnaround management?
Strong leadership is crucial for instigating cultural transformations within organizations, retaining talent, and maintaining operational continuity, especially during challenging times.
How does stakeholder engagement contribute to the success of healthcare turnaround initiatives?
Engaging stakeholders—including staff, patients, and suppliers—promotes collaboration and secures buy-in for proposed changes, enhancing the likelihood of successful implementation.
What should a strategic plan for healthcare turnaround management include?
A strategic plan should detail the desired outcomes and actionable steps necessary to achieve them, along with implementing streamlined decision-making processes and utilizing real-time analytics.
What is the significance of testing hypotheses in the turnaround process?
Testing hypotheses at every stage ensures maximum return on invested capital and allows for informed adjustments, which is essential for the success of turnaround efforts.
What strategies can organizations adopt to enhance operational efficiency in healthcare?
Strategies include streamlining processes, utilizing technology, implementing robust monetary management, optimizing the workforce, and adopting a patient-centric care approach.
How does streamlining processes improve healthcare performance?
Streamlining processes through comprehensive workflow analysis and Lean methodologies can eliminate waste and optimize patient flow, leading to improved operational efficiency.
What is the impact of technology on healthcare turnaround management?
Investing in advanced health information technology systems enhances data management, communication, and telemedicine services, boosting operational efficiency and fostering patient engagement.
Why is workforce optimization important in healthcare organizations?
Assessing staffing levels and skill sets, along with targeted training and development, enhances employee capabilities and service delivery, which is critical for operational success.
How does a patient-centric approach affect healthcare outcomes?
Transitioning to a patient-centered approach increases patient involvement in care plans, leading to better outcomes, increased satisfaction, and positively impacting operational metrics and economic performance.




