Overview
Cost reduction strategies for healthcare organizations are pivotal in enhancing operational efficiency. By conducting comprehensive financial assessments, implementing targeted initiatives, and integrating technology alongside data analytics, organizations can navigate fiscal challenges effectively. Analyzing fiscal landscapes and optimizing supply chains are essential components of this strategy.
Moreover, organizations must regularly evaluate their cost management practices to adapt to ongoing challenges. This proactive approach ensures that quality care is maintained while effectively managing expenses.
It is crucial for healthcare leaders to embrace these strategies to secure their financial future and continue delivering exceptional patient care.
Introduction
In the ever-evolving landscape of healthcare, organizations face significant financial pressures and operational challenges that demand immediate attention. To navigate these complexities, a thorough assessment of financial health and operational workflows is essential.
This article explores strategic approaches for healthcare organizations to enhance their financial stability through:
- Targeted cost reduction strategies
- The integration of technology
- The importance of regular evaluations
By embracing these methodologies, healthcare providers can not only survive but thrive in a competitive environment, ensuring both operational efficiency and improved patient outcomes.
Assess Financial Landscape and Operational Challenges
Healthcare organizations must initiate a thorough economic review to accurately evaluate their current fiscal landscape. This process involves a detailed analysis of revenue streams, expense categories, and operational workflows, supported by streamlined decision-making and real-time analytics. Key steps include:
- Fiscal Statement Analysis: Scrutinize income statements, balance sheets, and cash flow statements to uncover trends and anomalies that may influence economic health. As Ankit Jain, a senior analytics expert, emphasizes, effective financial statement analysis is crucial for understanding the underlying financial dynamics.
- Pricing Structure Assessment: Analyze fixed and variable expenses to identify where the majority of expenditures come from, facilitating focused expense reduction initiatives. Given the current challenges of high inflation and labor shortages, this evaluation is more critical than ever.
- Operational Workflow Assessment: Map out processes collaboratively to identify bottlenecks and inefficiencies that contribute to inflated costs, facilitating streamlined operations. Tackling these inefficiencies can assist entities in adjusting to the ongoing pressures in the healthcare sector. Our team supports a shortened decision-making cycle throughout the turnaround process, allowing decisive action to preserve business health.
- Benchmarking: Compare economic metrics against industry standards to evaluate performance and highlight areas ripe for improvement. We consistently track the effectiveness of our strategies via our client dashboard, which offers real-time business analytics to assess your business health persistently.
By performing this comprehensive evaluation, organizations can obtain essential insights into their economic well-being and operational difficulties. This foundational understanding is essential for implementing effective cost reduction strategies, particularly in the face of ongoing challenges such as high inflation and labor shortages. In fact, 93% of medical leaders are likely or very likely to invest in additional tools to enhance hiring efficiency, underscoring the urgency of these budget assessments.
Moreover, recent case studies show that tackling candidate dropouts in medical hiring has become vital, as inadequate communication and involvement have resulted in considerable challenges. By enhancing these areas, companies can improve overall hiring results, which directly contributes to their economic stability. The medical sector continues to adjust to the difficult circumstances arising from the pandemic, making these monetary assessments not just advantageous but crucial.
Implement Targeted Cost Reduction Strategies
To navigate the financial landscape effectively, medical organizations can implement cost reduction strategies that enhance operational efficiency and drive sustainable growth. Key approaches include:
- Operational Efficiency Improvements: Adopting Lean methodologies streamlines processes, eliminates waste, and significantly enhances productivity. This approach has been demonstrated to improve operational metrics across various medical environments. The integration of AI into healthcare, as highlighted in the case study "The Evolution of AI in Healthcare," illustrates how technological advancements can lead to better health outcomes and operational efficiency. Moreover, ongoing observation via real-time analytics enables entities to evaluate the impact of these enhancements and implement prompt modifications.
- Supply Chain Optimization: By negotiating improved terms with vendors and examining collective purchasing options, entities can effectively reduce procurement expenses. Strategies for supply chain optimization have shown significant savings, with statistics suggesting that efficient management can lower supply chain expenditures by up to 15% in 2025. In addition, employing real-time data analytics can further enhance decision-making, ensuring that entities can respond swiftly to market changes.
- Labor Cost Management: A thorough analysis of staffing levels and productivity metrics is essential for optimal workforce utilization. This can lead to decreases in overtime expenses and avoid unnecessary recruitment, ultimately enhancing the bottom line. Implementing a data-driven approach to monitor labor performance can help identify areas for improvement, ensuring that resources are allocated efficiently.
- Outsourcing Non-Core Functions: Outsourcing administrative tasks such as billing and coding to specialized firms can enhance efficiency. These companies frequently utilize technology to optimize operations, allowing medical institutions to concentrate on core strengths. The recent news about AI extending scheduling capabilities to telehealth services underscores how technology can improve operational efficiency in these outsourced functions. Continuous performance monitoring of these partnerships ensures they deliver the expected return on investment.
- Preventive Care Initiatives: Investing in preventive care programs can significantly lower long-term expenses related to chronic diseases and hospital admissions. By prioritizing preventive measures, institutions can enhance patient outcomes while reducing overall medical costs. Real-time analytics can track the effectiveness of these initiatives, allowing for adjustments that maximize their impact.
These approaches not only lead to prompt savings but also prepare medical entities for improved operational efficiency and adaptability in a swiftly changing sector. As Jason Allen, Head of MassMutual Catalyst Fund, noted, "Dock Health’s expansion into AI represents a pivotal moment for healthcare productivity. This innovation aligns perfectly with the growing demand for scalable, value-based care solutions.
Utilize Technology and Data Analytics for Cost Management
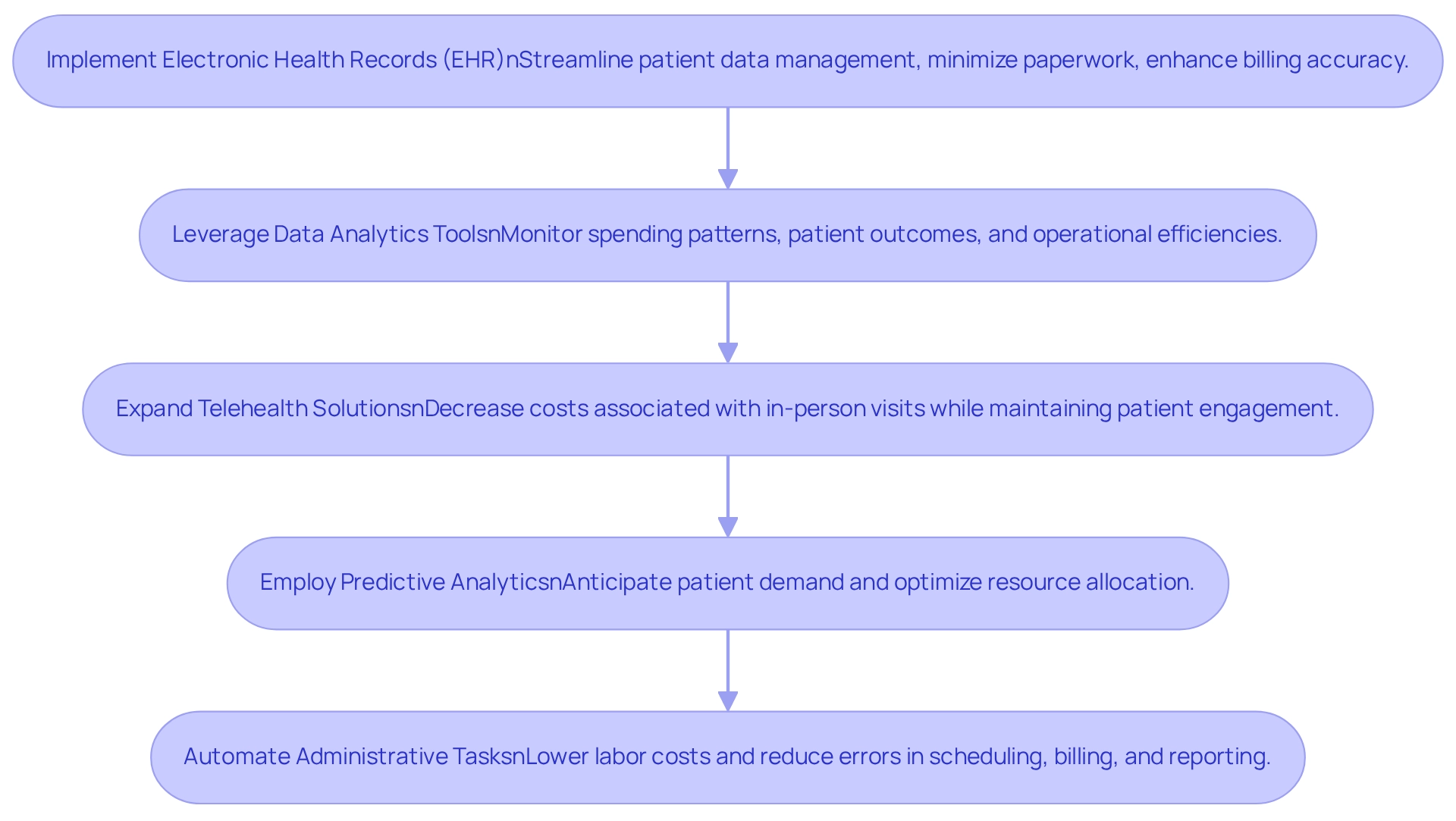
Healthcare organizations must integrate technology and data analytics as essential elements of their cost reduction strategies. Key actions include:
- Implementing Electronic Health Records (EHR): EHR systems streamline patient data management, minimize paperwork, and enhance billing accuracy.
- Data Analytics Tools: Leverage analytics to monitor spending patterns, patient outcomes, and operational efficiencies, facilitating informed decision-making.
- Telehealth Solutions: Expand telehealth services to decrease costs associated with in-person visits while maintaining patient engagement.
- Predictive Analytics: Employ predictive models to anticipate patient demand and optimize resource allocation, thereby curtailing unnecessary expenditures.
- Automation of Administrative Tasks: Invest in automation tools for scheduling, billing, and reporting to lower labor costs and reduce errors.
By embracing these technologies, organizations can realize significant savings through effective cost reduction strategies while simultaneously enhancing the quality of care.
Evaluate and Adapt Cost Reduction Practices Regularly
To achieve and sustain financial stability, healthcare entities must continuously evaluate and enhance their cost reduction strategies. This can be effectively accomplished through the following approaches:
- Performance Metrics Monitoring: Implement key performance indicators (KPIs) to assess the effectiveness of expense reduction initiatives. Regular tracking of these metrics allows organizations to pinpoint areas for improvement and measure the impact of their strategies. A study involving 76 general internists revealed that most physicians were unaware of their performance scores, underscoring the critical need for effective performance metrics monitoring in expense management. Moreover, utilizing real-time analytics can provide immediate insights into business health, enabling timely adjustments to strategies.
- Regular Monetary Reviews: Conduct quarterly assessments to uncover emerging challenges and opportunities for cost savings. These evaluations are essential for adapting to the ever-changing healthcare environment and ensuring that monetary practices remain robust. The Agency for Healthcare Research and Quality emphasizes the significance of performance-based provider payment arrangements, highlighting the importance of regular evaluations in aligning financial practices with performance metrics. Streamlined decision-making processes during these reviews can facilitate quicker responses to identified issues.
- Stakeholder Feedback: Actively engage staff and management in discussions regarding cost management practices. John Brownstein notes that focusing on impactful areas rather than distractions is essential for innovation. Collecting insights from different tiers of the entity fosters a culture of ongoing enhancement and creativity. This relationship-building is vital for operationalizing turnaround lessons and ensuring that all voices contribute to strategic planning.
- Market Analysis: Stay informed about industry trends and competitor strategies. Understanding the market landscape enables entities to proactively modify their practices, ensuring they remain competitive and efficient. Tracking member satisfaction and complaint rates is crucial for payers to identify service shortcomings, as satisfied members are more likely to stay with their health plans. Continuous monitoring of market dynamics can inform strategic decisions and enhance overall performance.
- Training and Development: Invest in training programs that equip staff with the skills necessary to identify and implement cost-saving measures. A well-trained workforce is essential for sustaining effective expenditure management practices. By nurturing a culture of learning and adjustment, entities can more effectively apply insights gained from previous initiatives.
By committing to consistent assessment and modification, medical institutions can ensure that their cost reduction strategies are not only efficient but also aligned with their overarching financial goals. This proactive approach is crucial in navigating the complexities of the healthcare industry, especially as organizations face increasing pressure to manage expenses while maintaining quality care. Furthermore, understanding patient perspectives, as highlighted in the case study on the need for further research, is vital in evaluating the impact of cost reduction strategies on patient care and outcomes.
Conclusion
Healthcare organizations stand at a critical juncture, where the integration of strategic financial assessments and operational improvements can lead to enhanced stability and resilience in a challenging environment. By thoroughly assessing their financial landscape and operational workflows, organizations can identify key areas for improvement, ensuring they are prepared to tackle the unique challenges posed by rising costs and evolving industry demands.
Implementing targeted cost reduction strategies, such as improving operational efficiency and optimizing supply chains, not only streamlines processes but also fosters sustainable growth. The adoption of technology, including electronic health records and data analytics, further empowers organizations to make informed decisions that enhance both financial outcomes and patient care quality.
Moreover, the commitment to regular evaluations and adaptations of cost management practices ensures that healthcare providers remain agile and responsive to the ever-changing landscape. By actively engaging stakeholders and investing in continuous learning, organizations can cultivate a culture of innovation that drives long-term success.
In conclusion, the proactive embrace of these strategies positions healthcare organizations not just to survive but to thrive in an increasingly competitive sector. By prioritizing financial health and operational excellence, healthcare providers can ultimately improve patient outcomes while securing their financial future. Now is the time for organizations to take decisive action and implement these vital methodologies to achieve lasting impact and success.
Frequently Asked Questions
What is the purpose of conducting a thorough economic review in healthcare organizations?
The purpose is to accurately evaluate the current fiscal landscape by analyzing revenue streams, expense categories, and operational workflows, supported by streamlined decision-making and real-time analytics.
What are the key steps involved in the economic review process?
The key steps include Fiscal Statement Analysis, Pricing Structure Assessment, Operational Workflow Assessment, and Benchmarking.
How does Fiscal Statement Analysis contribute to understanding economic health?
It involves scrutinizing income statements, balance sheets, and cash flow statements to uncover trends and anomalies that may influence economic health, which is crucial for understanding financial dynamics.
Why is Pricing Structure Assessment important, especially in the current economic climate?
It helps identify the sources of fixed and variable expenses, facilitating focused expense reduction initiatives, which is critical due to challenges like high inflation and labor shortages.
What is the goal of Operational Workflow Assessment?
The goal is to map out processes collaboratively to identify bottlenecks and inefficiencies that contribute to inflated costs, thereby facilitating streamlined operations.
How does Benchmarking assist healthcare organizations?
Benchmarking compares economic metrics against industry standards to evaluate performance and highlight areas for improvement, while also tracking the effectiveness of strategies through real-time business analytics.
What insights can organizations gain from performing a comprehensive evaluation?
Organizations can obtain essential insights into their economic well-being and operational difficulties, which are vital for implementing effective cost reduction strategies.
What recent trends emphasize the urgency of budget assessments in healthcare?
The ongoing challenges such as high inflation and labor shortages have led 93% of medical leaders to consider investing in tools to enhance hiring efficiency, highlighting the need for budget assessments.
Why is addressing candidate dropouts in medical hiring important?
Inadequate communication and involvement have led to significant challenges in hiring, so improving these areas can enhance overall hiring results and contribute to economic stability.
How has the pandemic affected the need for monetary assessments in the medical sector?
The medical sector continues to adjust to difficult circumstances arising from the pandemic, making monetary assessments crucial for navigating these challenges.




