Overview
Cost reduction strategies in hospitals aimed at enhancing efficiency prioritize the optimization of healthcare staff through targeted training, fostering increased physician engagement, analyzing patient flow, leveraging evidence-based standards of care, and bundling contracts with suppliers. This article underscores the significance of comprehensive training programs and data analytics in bolstering operational efficiency. Moreover, it highlights how physician involvement and standardized practices not only lead to improved patient outcomes but also contribute to substantial cost savings.
Introduction
In the dynamic landscape of healthcare, organizations are continuously seeking innovative strategies to enhance operational efficiency and patient care. From optimizing staff training to leveraging data analytics for improved patient flow, the focus is on creating a more responsive and effective system. By embracing evidence-based practices and standardizing contracts, healthcare providers can not only reduce costs but also improve outcomes. This comprehensive approach highlights the importance of collaboration, continuous education, and strategic decision-making in fostering a healthcare environment that prioritizes both staff engagement and patient satisfaction. As the industry evolves, these strategies are essential for navigating the challenges ahead and ensuring sustainable growth.
Optimize Healthcare Staff Through Training and Development
Implementing comprehensive training programs for healthcare staff is crucial for enhancing skills and operational efficiency. Continuous learning about the latest medical practices, technology application, and protocols for individuals is essential. Cross-training staff not only fosters role flexibility but also ensures optimal coverage during peak times or staff shortages, directly impacting hospital efficiency. For instance, recent initiatives have demonstrated that hospitals utilizing cross-training strategies see a significant rise in staff performance and care quality, backed by the reality that training packages created by NHSBT are among the most commonly downloaded resources on the ATTC network website.
Moreover, blended learning methods, which merge online courses with practical training, accommodate various learning styles and greatly enhance information retention. This method is exemplified by the development of e-learning modules for NHS staff, which aim to provide standardized training that enhances both theoretical knowledge and practical skills necessary for advanced therapy delivery. Regular assessments are vital for identifying skill gaps; for instance, they can reveal specific areas where staff may need additional training, thereby allowing for tailored programs that effectively meet patient needs. Such initiatives not only streamline operations but also contribute to long-term cost reduction strategies in hospitals, particularly through a standardized national approach for NHS staff training that enhances efficiency and reduces overhead.
Encourage Increased Physician Engagement
To enhance physician involvement, healthcare organizations must implement strategies that foster collaboration and open communication. Frequent gatherings focused on healthcare approaches can stimulate discussions among doctors, while feedback systems facilitate effective issue resolution. Recognition programs that honor physician contributions further encourage engagement. Involving physicians in decision-making processes regarding clinical protocols and operational changes cultivates a sense of ownership and accountability. Moreover, providing resources for professional growth and wellness programs can mitigate burnout, ultimately boosting both engagement and productivity.
Statistics indicate that organizations with high physician involvement experience a 20% improvement in care outcomes. Additionally, it is noted that eight partners can leverage this purpose to select content based on restricted data, underscoring the importance of targeted engagement strategies. A case study involving Practice Fusion, a cloud-based EHR system designed for small to medium-sized medical practices, illustrates how its user-friendly interface and integrated e-prescribing enhance clinical efficiency and user engagement. This exemplifies the tangible benefits of collaborative practices and technology in improving operational efficiency. By prioritizing these strategies, medical organizations can cultivate an environment where physicians feel valued and empowered, leading to enhanced care and organizational success. Simon Lorenz, Ph.D., Co-Founder, emphasizes the importance of understanding the business side of healthcare, asserting that effective engagement is essential for achieving better outcomes.
Analyze and Adjust Services for Optimal Patient Flow
Examining client flow necessitates a thorough assessment of the complete individual journey, from admission to discharge. By leveraging data analytics, hospitals can identify bottlenecks and inefficiencies that can be addressed through cost reduction strategies. For instance, implementing triage systems enables prioritization of care based on urgency, while optimized scheduling can significantly decrease wait times for procedures.
Moreover, frequent assessments of client flow metrics, combined with tactical modifications to staffing levels, guarantee that resources are distributed efficiently. Furthermore, promoting improved communication between departments is essential for implementing cost reduction strategies, as it can streamline operations and enhance throughput for those receiving care.
With the client flow management market projected to reach $6.76 billion by 2027, the integration of data analytics is crucial for optimizing hospital efficiency and developing cost reduction strategies to enhance outcomes. Significantly, a 2022 survey conducted by the Press Ganey consulting firm discovered that 63% of individuals reported waiting over 30 minutes to see a physician during their last appointment, highlighting the urgency of tackling flow issues.
Additionally, the growing demand for skilled healthcare data analysts underscores the importance of data-driven decision-making in hospitals. A relevant case study involves AI systems developed for automated image segmentation in radiology, which have shown significant improvements in operational efficiency, demonstrating the potential of technology to enhance patient flow management.
Leverage Evidence-Based Standards of Care
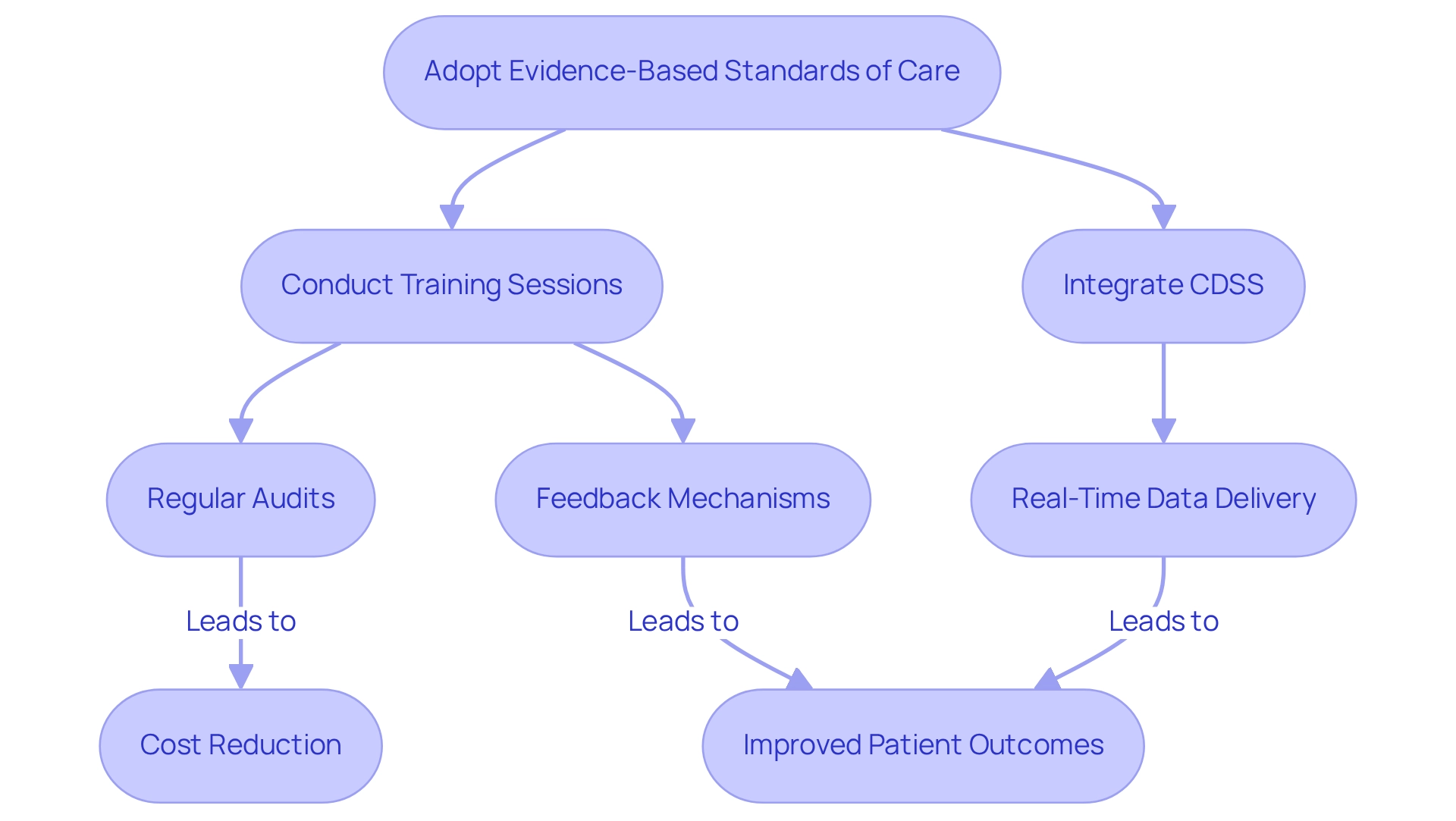
Healthcare institutions must adopt evidence-based standards of practice to align treatments and procedures with the latest clinical guidelines. This approach includes:
- Conducting regular training sessions for staff on updated protocols.
- Integrating clinical decision support systems (CDSS) that deliver real-time data to healthcare providers.
By standardizing treatment processes, hospitals can implement cost reduction strategies to minimize variations in treatment. This not only improves outcomes for individuals but also decreases expenses associated with unnecessary tests and procedures. For instance, studies indicate that implementing evidence-based practices can lead to a 15% reduction in length of stay and a 12% decrease in mortality rates.
Regular audits and feedback mechanisms are essential to ensure adherence to these standards, fostering a culture of continuous improvement and accountability. Moreover, continuous investigation into the implementation of evidence-based information via electronic systems is crucial for enhancing safety and quality of service.
As Marita G. Titler, Ph.D., R.N., F.A.A.N., emphasizes, "The role of leaders, clinicians, publishers, and educators is vital in improving the current state of evidence-based practice." By acknowledging the professional duties of all parties involved, including leaders and clinicians, medical organizations can significantly enhance the effectiveness of evidence-based practices and improve cost reduction strategies in hospitals. This ultimately results in better patient outcomes and operational efficiency.
Additionally, the case study titled 'Professional Responsibility in Advancing Evidence-Based Practice' highlights key actions needed to clarify the distinctions between quality improvement, implementation science, and research, further supporting the argument for a structured approach to evidence-based care.
Bundle and Standardize Contracts
Bundling and standardizing contracts with suppliers and service providers emerge as effective cost reduction strategies within hospitals, particularly in light of the financial pressures they face. Recent reports indicate that health systems encountered financial difficulties during Q2 last year, primarily due to the suspension of elective surgeries. This situation underscores the urgent need for cost reduction strategies in hospitals. By negotiating comprehensive agreements that encompass multiple services or products, these organizations can leverage their purchasing power to secure more favorable rates. Research demonstrates that medical systems implementing cost reduction strategies through bundling approaches have reported substantial savings, with some achieving reductions of up to 15% in procurement expenses.
Standardizing contract terms not only streamlines the negotiation process but also enhances compliance with regulatory obligations, thereby minimizing the risk of costly penalties. A centralized contract management system is vital in this context, enabling organizations to effectively track contract performance and manage renewals. This ensures that medical providers consistently receive optimal value for their expenditures.
Moreover, the case study on Member Self-Direction in Medical Choices illustrates how engaging members in selecting participating facilities can enhance satisfaction and program effectiveness. This approach aligns procurement strategies with broader organizational goals and emphasizes the importance of services being conducted with patients, rather than merely to them. Such engagement can lead to improved financial outcomes and the adoption of cost reduction strategies in hospitals, contributing to a more sustainable medical model.
In addition, expert insights highlight the necessity of focusing on impactful innovations rather than transient trends. As Michael Restuccia noted, successful projects require a combination of ‘people, process, and technology.’ This reinforces the significance of strategic procurement practices in achieving sustainable growth within the healthcare sector.
Conclusion
Enhancing operational efficiency and patient care in healthcare organizations necessitates a strategic approach. Prioritizing comprehensive staff training equips teams with essential skills, while cross-training and blended learning enhance flexibility and outcomes.
Engaging physicians through collaboration and open communication is vital. Involving healthcare professionals in decision-making fosters ownership and significantly elevates patient care.
Utilizing data analytics to analyze patient flow enables hospitals to identify bottlenecks and streamline processes, thereby reducing wait times and improving satisfaction. Embracing evidence-based standards of care aligns practices with clinical guidelines, minimizing treatment variations and enhancing safety.
Moreover, bundling and standardizing contracts with suppliers can lead to substantial cost savings, facilitating better resource management in a challenging financial landscape.
In summary, integrating strategies such as staff training, physician engagement, data-driven decision-making, evidence-based practices, and strategic procurement will cultivate a healthcare environment that prioritizes both operational efficiency and patient satisfaction. Embracing these approaches is essential for navigating future challenges and achieving lasting success in the healthcare sector.
Frequently Asked Questions
Why are comprehensive training programs important for healthcare staff?
Comprehensive training programs are crucial for enhancing skills and operational efficiency, ensuring that staff are continuously learning about the latest medical practices, technology applications, and protocols.
What is the benefit of cross-training healthcare staff?
Cross-training fosters role flexibility and ensures optimal coverage during peak times or staff shortages, which directly impacts hospital efficiency and improves staff performance and care quality.
How do blended learning methods enhance training for healthcare staff?
Blended learning methods combine online courses with practical training, accommodating various learning styles and greatly enhancing information retention.
What role do regular assessments play in staff training?
Regular assessments help identify skill gaps, allowing for tailored training programs that effectively meet patient needs and streamline operations.
How can physician involvement improve healthcare outcomes?
High physician involvement leads to a 20% improvement in care outcomes by fostering collaboration, open communication, and encouraging physicians to participate in decision-making processes.
What strategies can healthcare organizations use to enhance physician engagement?
Strategies include frequent gatherings for discussions, feedback systems for issue resolution, recognition programs for contributions, and providing resources for professional growth and wellness programs.
What are the benefits of using technology, such as EHR systems, in healthcare practices?
Technology like cloud-based EHR systems enhances clinical efficiency and user engagement, demonstrating the benefits of collaborative practices in improving operational efficiency.
How can understanding the business side of healthcare impact engagement and outcomes?
Understanding the business side is essential for effective engagement, which is crucial for achieving better healthcare outcomes, as emphasized by experts in the field.




