Introduction
Understanding the intricate relationship between cost and price is essential in cost accounting. Cost represents the total expenses incurred in creating goods or services, while price is the value attached to a product or service for sale to the customer. These concepts play a pivotal role in shaping business strategies and operational decisions.
Recognizing the difference between cost and price fosters a cost-aware culture within organizations, influencing every aspect of operations. Recent trends in operational efficiency, such as the use of AI in various industries, highlight the need for transparency in financial management. Cost accounting systems have adapted to provide more than just a record of expenses; they offer a framework to control costs effectively and optimize long-term organizational efficiency.
The strategic role of cost accounting is further emphasized in healthcare, where it helps providers deliver high-quality care while managing expenses. By embracing technology and data analytics, healthcare systems can streamline operations, reduce costs, and improve patient outcomes. However, challenges and limitations exist in achieving price transparency, including technological hurdles, consumer awareness, and privacy concerns.
Despite these challenges, cost accountants and business leaders must develop strategies to leverage the benefits of price transparency while addressing limitations. Real-world examples in various industries demonstrate how cost accounting informs decision-making and drives superior performance and sustainable growth.
Understanding the Terminology: Cost vs. Price
Understanding the intricate relationship between cost and price is a cornerstone of effective cost accounting. While cost encapsulates the total amount spent on the creation of goods or services, including both direct expenses such as materials and labor and indirect ones like overhead, price is the value attached to a product or service for sale to the customer. These two concepts are not just academic; they play a pivotal role in shaping business strategies and operational decisions.
In the realm of cost accounting, recognizing the difference between cost and price is more than a theoretical exercise; it's about fostering a cost-aware culture within an organization. By integrating cost as a non-functional requirement, akin to system availability or reliability, businesses ensure that financial considerations become an intrinsic part of the product development cycle. It's a shared responsibility that extends beyond the finance team, influencing every aspect of operations.
Recent trends in operational efficiency underscore this shift, with industries like software, professional services, health care, and financial services increasingly incorporating technologies such as AI to enhance productivity and safeguard margins. Companies are keenly aware of the need for transparency in financial management to avoid unexpected expenditures, as evidenced by initiatives like Microsoft Cost Management's efforts to provide clearer insights into cloud spending.
In light of these industry movements, cost accounting systems have adapted to provide more than just a record of expenses. They offer a framework to control costs effectively, as seen in various sectors like steel production, where multiple departments necessitate meticulous cost tracking. The objective is not only to monitor but also to optimize costs for long-term organizational efficiency, leading to substantial savings over time.
The strategic role of cost accounting is further highlighted by the Food Dollar Series, which delineates the consumer's food expenditure across different segments of the food-supply chain. This granular view into the allocation of costs underscores the importance of understanding the full financial picture, from immediate costs to long-term economic benefits.
Healthcare Costs and Quality: An Analytical Perspective
Cost accounting is a critical tool for healthcare providers seeking to deliver high-quality care while managing expenses. A compelling case study reveals how a large physician organization was burdened by laborious manual processes that absorbed the time of three business analysts each week, just to produce a key management report. By shifting away from manual reporting and embracing technology such as automation, healthcare systems can streamline operations and reduce costs.
In another instance, Pacific Steel, a self-insured company with approximately 900 employees, faced opaque healthcare costs that skyrocketed with traditional provider networks. The company's executives chose to break away from a major insurer, opting for a smaller administrator that promised greater transparency. Utilizing reference-based pricing, they began paying for health care services based on Medicare rates, resulting in substantial cost savings.
This strategic move was facilitated by a deep analysis of insurance claims data, highlighting the power of cost accounting.
The inefficiencies of quality measurement in healthcare, described as 'horribly inefficient' and costing billions, further underscore the need for better data management. Without a single source to track care quality, hospitals must juggle various types of data, leading to significant administrative overhead.
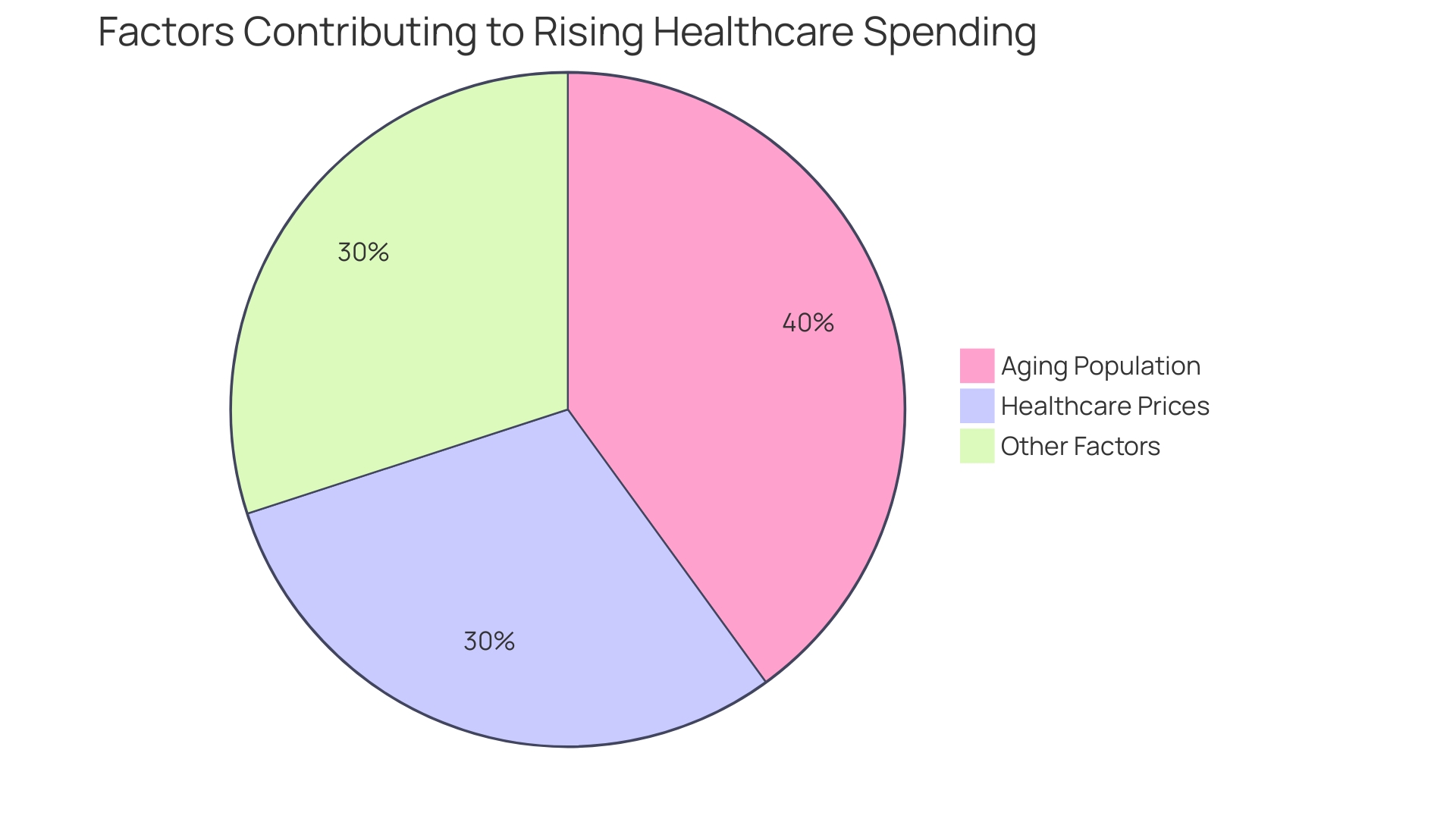
Moreover, statistics show that national health expenditures in the U.S. reached a staggering $4.5 trillion in 2022, with healthcare costs continuing to climb. This emphasizes the urgency for healthcare systems to adopt cost accounting practices to identify inefficiencies and control spending.
The challenges of equipment management in health systems, where lack of organization leads to unpredictable costs, can be addressed by standardizing clinical engineering processes. This not only streamlines operations but also improves safety and reduces expenses. An organized approach to managing medical device inventories can prevent resource wastage and provide health systems with a clearer financial picture.
Ultimately, the integration of cost accounting practices in the healthcare industry can lead to enhanced patient outcomes and operational efficiencies. By leveraging data analytics, healthcare leaders can make informed decisions, ensuring the sustainability of their organizations in a landscape of rising costs and complex regulations.
Case Study: The Impact of Transparency on Healthcare Costs
The quest for healthcare price transparency has sparked a movement to peel back the layers of opacity surrounding the cost of medical services. With over 50 billion claims data points at our disposal, representing nearly three-quarters of U.S. claims, we're at the forefront of deciphering the intricacies of healthcare pricing. It's a confounding puzzle, with no single pricing blueprint across insurers and hospitals, but rather a labyrinth of billing conventions that muddy the waters of service costs.
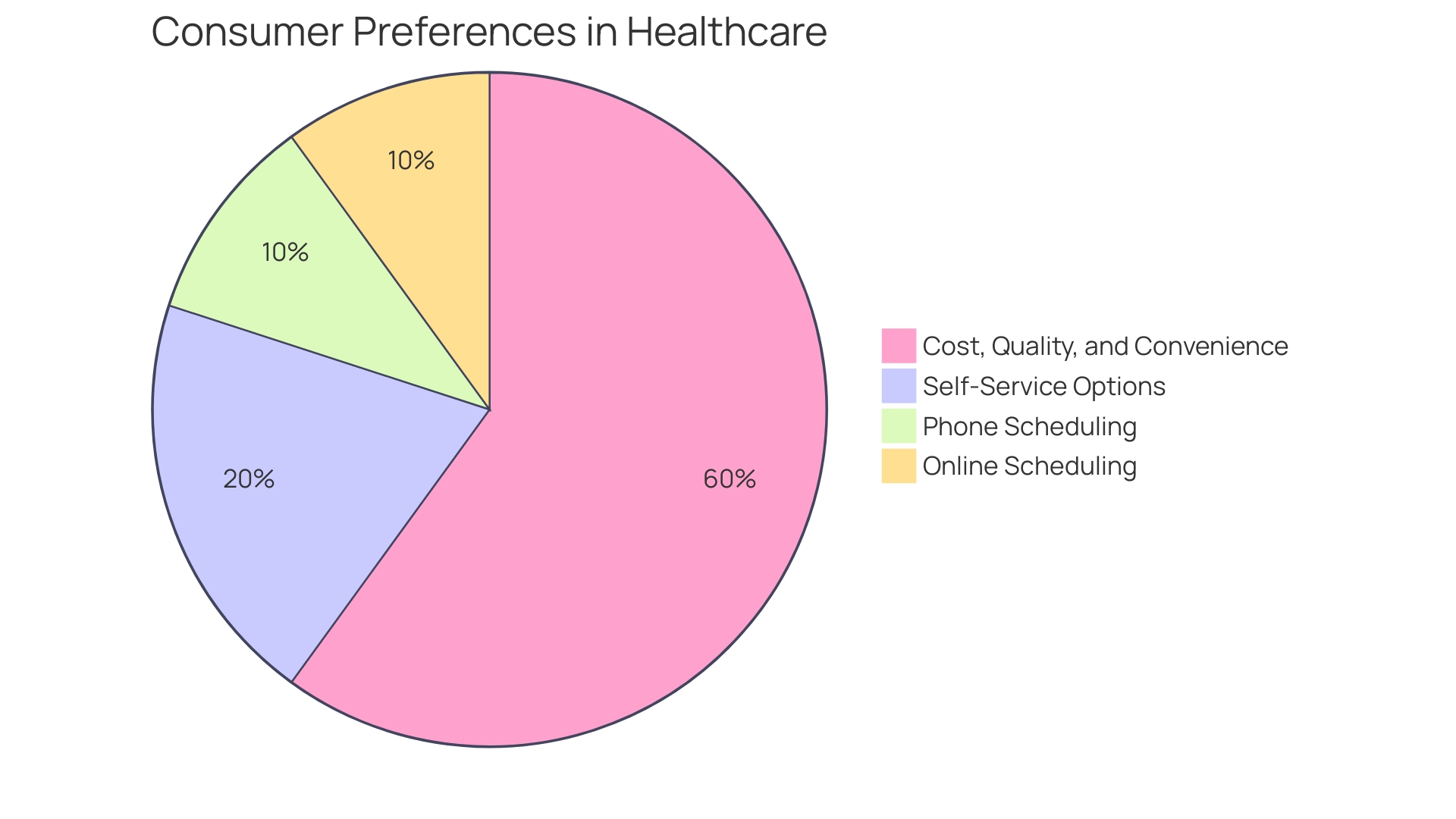
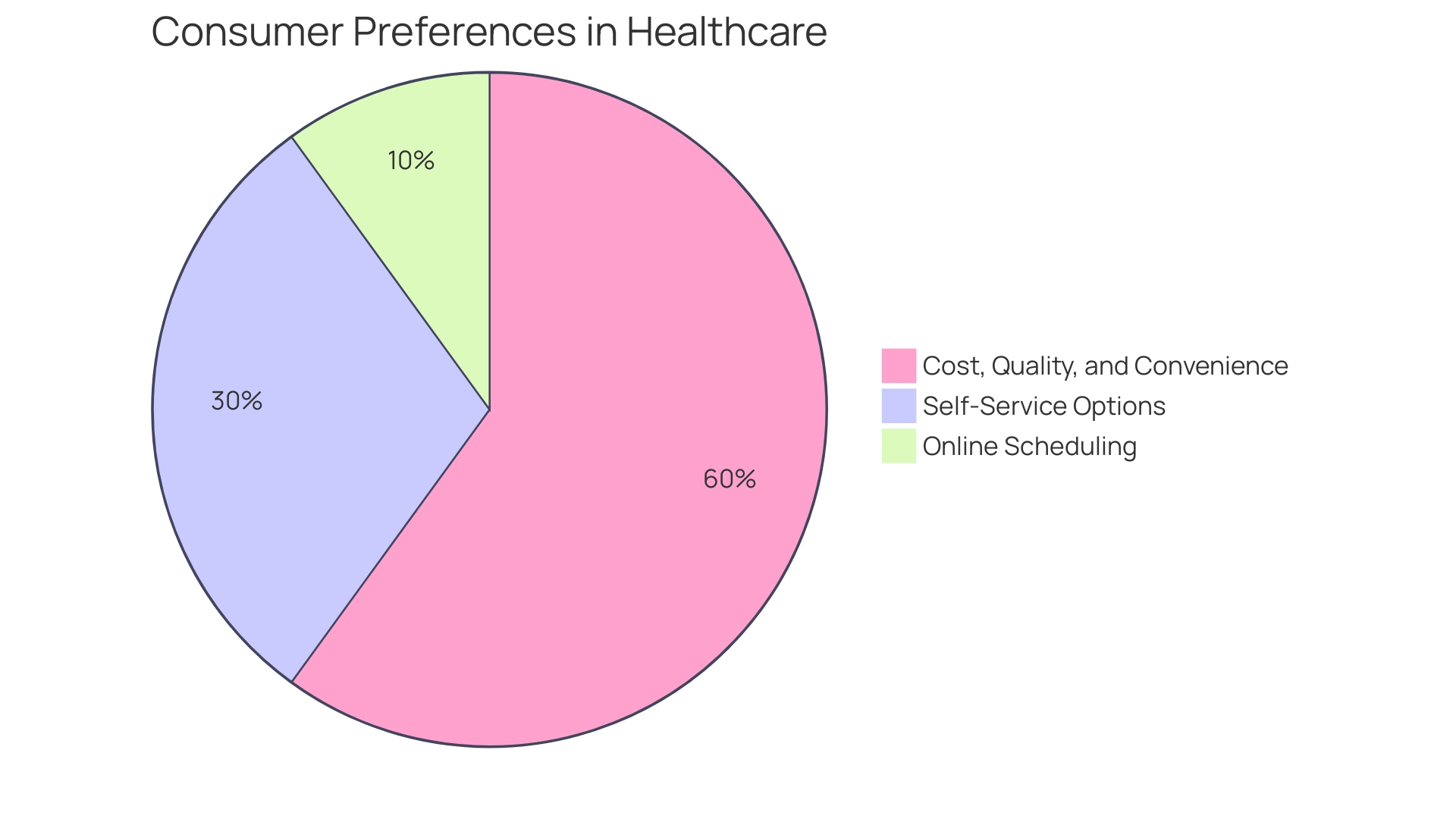
Despite initial optimism, the reality is that the anticipated consumer-driven 'shopping' for healthcare services hasn't materialized. Even with tools to compare costs, a mere 3-4% of patients engage with these digital resources for procedures, while a staggering 70% use them to select new physicians. This suggests that when it comes to specific medical procedures, patients continue to rely on their doctors' recommendations rather than hunting for cost savings.
The Hospital Price Transparency rule, enacted in January 2021 by the CMS, mandated hospitals to disclose prices for 200 shoppable services in a user-friendly format. Compliance, however, has been patchy. A significant number of hospitals have yet to fully adhere to the rule, and as such, the potential for price transparency to catalyze competition and consumerism in healthcare remains unfulfilled.
To turn the tide, the data must not only be accessible but also actionable. This involves harmonizing the data across services and hospitals and presenting it in a format that is easy for consumers, industry, and researchers to navigate. An information campaign to raise public awareness of the availability and advantages of price transparency could be a pivotal step towards spurring consumers to make cost-conscious healthcare choices.
The goal is clear: to leverage price transparency to drive down healthcare costs through informed decision-making and market competition.
Federal Regulations and Hospital Price Transparency
Federal regulations and policies have recently made significant strides towards enhancing price transparency in healthcare. A pivotal moment came with the introduction of the Hospital Price Transparency rule by the Centers for Medicare and Medicaid Services (CMS), which took effect in January 2021. This mandate requires hospitals to disclose prices for 200 shoppable services in a format that machines can read, directly on their websites.
Noncompliance carries financial consequences.
Despite these efforts, the labyrinth of healthcare pricing remains complex. The vastness of the data is staggering, with over 50 billion individual claims processed, highlighting the lack of a standardized structure in how hospitals and insurers negotiate prices. This complexity necessitates robust data engineering to make sense of the information, as the variety of billing methods, grouping, and payment conventions greatly affect the final costs of services.
The expectation that consumers would use this data to 'shop' for more affordable care has not materialized. Studies, including those by JAMA and Harvard, reveal that only a small fraction of patients — about 3-4% — utilize digital tools to find lower-cost service locations. Contrastingly, digital tools are much more frequently employed when seeking a new doctor, with over 70% of patients turning to them.
Health insurance companies have introduced price-lookup tools tailored to individual plans, but these often provide average costs rather than actual billed amounts. A Health Affairs paper argued that actual prices need to be disclosed to hold providers accountable, as estimates are of limited use to consumers and employers.
The push for transparency aims to foster competition and provide policymakers, researchers, and consumers with actionable data. For transparency to have a meaningful impact, it must be consistent and accessible. However, the reality of consumption patterns and plan designs offers little incentive for patients to seek cost-saving alternatives.
In summary, while federal regulations have laid the groundwork for increased transparency in healthcare pricing, the interplay between complex data structures, consumer behavior, and the actual utility of the disclosed information poses ongoing challenges for hospitals in aligning their cost accounting practices with these regulations.
Consumer Benefits of Price Transparency
Price transparency in healthcare has come a long way, but it's clear that simply having data available doesn't equate to consumers actively using it to make cost-effective decisions. Despite the availability of over 50 billion individual claims data, representing a staggering 75% of all U.S. claims, the utilization of this data by consumers for shopping for more affordable medical procedures remains remarkably low. Studies have indicated that only 3-4% of patients use digital tools to seek out lower-cost locations for medical procedures.
This contrasts sharply with the 70% who use these tools to find new doctors, suggesting a complex relationship between price transparency and consumer behavior.
The healthcare industry's efforts to provide price transparency, such as the Trump administration's price transparency rule for hospitals, have encountered challenges. While some hospitals have been acknowledged for their full compliance and transparent posting of prices, analysis reveals that many still do not meet the requirements, leaving consumers without the complete information they need.
The concept of price transparency extends beyond healthcare. The idea that consumers benefit from the ability to compare costs and make informed decisions is exemplified in everyday scenarios, like cereal shopping, where price and nutritional information is readily available. This idea is reinforced by the argument that well-functioning markets require complete and accurate information about prices and quality.
Even in industries where price transparency is well-established, the impact on cost accounting practices is significant. Accurate and timely information about prices allows for more effective management of expenses and supports the efficient operation of markets. As businesses navigate the complexities of price disclosure, it's crucial to recognize the role of transparency in shaping consumer choices and driving competition.
The implications for cost accounting are profound. With actual prices becoming more accessible, businesses can no longer rely on estimates but must instead focus on the accountability that comes with listed prices. This shift emphasizes the need for a nuanced approach to pricing strategies, taking into account not just the cost of services but also the consumer perspective and their actual decision-making processes.
Challenges and Limitations in Achieving Price Transparency
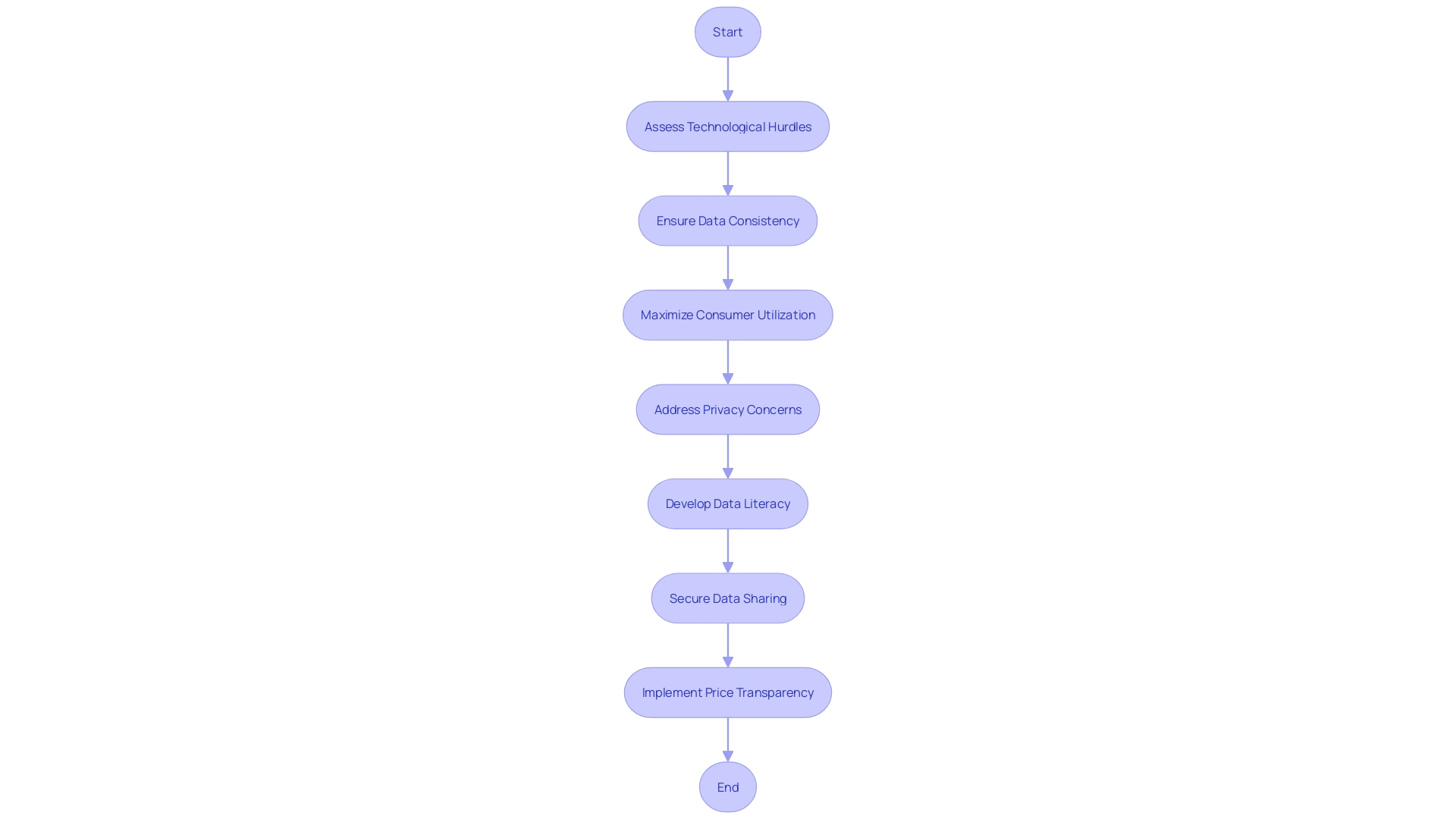
Implementing price transparency presents a complex set of challenges that organizations must navigate carefully. The transition to transparent pricing can be fraught with technological hurdles, such as the need for machine-readable formats that meet specific regulatory standards. As evidenced by the new CMS rules requiring hospitals to post prices for certain services, the shift towards transparency is a significant step, but it comes with its own set of difficulties.
For instance, ensuring data consistency across services and adherence to the Hospital Price Transparency rule demands rigorous compliance efforts.
Moreover, there are concerns about the actual utilization of this price information by consumers. Despite the potential for price transparency to foster competition and reduce healthcare spending, its effectiveness hinges on consumer awareness and the willingness to compare options. It's not enough to simply provide data; it must be actionable and comprehensible to truly influence consumer behavior and drive cost-effective decisions in healthcare.
The challenge of balancing privacy with transparency cannot be overstated. Data sharing involves navigating the tightrope between openness and privacy protection, which can be particularly sensitive in healthcare. To forge ahead, policymakers and industry leaders might look towards initiatives that enhance data literacy and securely expand data sharing, particularly in pivotal sectors such as healthcare and education.
These challenges are not insurmountable, but they require a concerted effort from all stakeholders involved. Cost accountants and business leaders must be at the forefront of developing strategies that recognize and address these limitations while leveraging the undeniable benefits of price transparency.
Real-World Examples: Comparing Costs and Quality
Delving into the realm of cost accounting reveals a compelling narrative of how businesses navigate the delicate balance between managing expenses and maintaining quality. It's through the meticulous scrutiny of various industry practices that we can glean insights into the art of cost efficiency. For instance, in manufacturing, companies are often confronted with the challenge of setting prices that reflect both the cumulative costs of production and a margin for profitability.
This delicate equilibrium is influenced by the interplay of supply and demand, ensuring that the market price gratifies both producer and consumer needs.
In the retail sector, the focus shifts to the value lines, where retailers exert considerable effort to minimize costs without compromising the quality that customers have come to expect. This pursuit often results in a myriad of products experiencing a decline in price, directly benefiting those most impacted by economic fluctuations. The narrative here is not one of retailers being vilified but rather celebrated for their dedication to delivering value amidst a cost-of-living crisis.
The service industry, too, offers compelling case studies, particularly in the application of cost-benefit analysis for operational changes. This involves a simplified yet effective approach that includes evaluating the time investment required from various stakeholders, from staff and management to customers or patients. The goal is to streamline policies without imposing undue burdens, thereby enhancing efficiency and organizational effectiveness.
Moreover, cost accounting transcends the mere tracking of expenses; it embodies a strategic tool that informs decision-making. By employing standard cost accounting, for example, firms can compare actual expenditures against standard costs under typical operating conditions, pinpointing areas for potential savings and process optimization.
The essence of cost accounting lies in its ability to provide clarity and transparency, enabling stakeholders to understand the assumptions that underpin financial models and make informed decisions. This is evident in the meticulous documentation of assumptions in cost model validation, which serves as a foundation for financial clarity and accountability.
Through these industry-specific examples, CFOs and cost accountants can extract actionable insights to refine their decision-making processes, ultimately propelling their businesses toward superior performance and sustainable growth.
Conclusion
Understanding the relationship between cost and price is crucial in cost accounting. It fosters a cost-aware culture and influences all aspects of operations. Cost accounting systems have evolved to optimize efficiency and drive sustainable growth.
Real-world examples demonstrate its impact in various industries.
In healthcare, cost accounting plays a critical role in delivering high-quality care while managing expenses. Embracing technology and data analytics can streamline operations, reduce costs, and improve patient outcomes.
However, challenges exist in achieving price transparency, including technological hurdles, consumer awareness, and privacy concerns. Despite these challenges, cost accountants and business leaders must develop strategies to leverage the benefits of price transparency while addressing limitations.
Federal regulations have made strides in enhancing price transparency in healthcare, but aligning cost accounting practices remains a challenge.
Price transparency has the potential to empower consumers to make cost-effective decisions. Efforts should focus on making the data actionable and raising public awareness.
Implementing price transparency presents challenges, including technological hurdles, consumer awareness, and privacy concerns. Strategies must address these challenges while leveraging the benefits.
Delving into cost accounting reveals real-world examples of businesses navigating the balance between managing expenses and maintaining quality. Extracting actionable insights allows CFOs and cost accountants to refine decision-making processes and drive sustainable growth.
In conclusion, understanding the difference between cost and price is crucial in cost accounting. Embracing technology, leveraging data analytics, and addressing the challenges of price transparency can optimize efficiency, control costs, and drive sustainable growth.




